The fatty acid binding protein (FABP) family is instrumental in adipocyte biology and contributes to metabolic disorders such as obesity. Recent evidence suggests these proteins may also play a role in cancer through affecting fatty acid metabolism, PPARG signaling, or other pathways. We analyzed several microarray patient datasets and found that increases in FABP5 expression in multiple myeloma (MM) cells correlates with poor overall survival and shorter relapse free survival (Zhan et al. Blood, 2006., Mulligan et al. Blood, 2006., Carrasco et al. Cancer Cell, 2006). Interestingly, when MM patients are classified into molecular subtypes, MM cells from "proliferative" (most aggressive) patient subgroups have the highest expression of FABP5 (Zhan et al. 2006). Additionally, MM cells from relapsed patients have increased expression of FABP5 versus newly-diagnosed patients (Chng et al. Cancer Research, 2007). Since FABPs have been shown to compensate for each other, and the Zhen dataset revealed that FABP4 and FABP5 expression are significantly correlated in MM cells, we next investigated targeting both FABP4 and FABP5 in myeloma preclinically.
We tested two well-known FABP inhibitors, BMS309403 and SBFI-26 (which are mainly inhibitors of FABP4 and FABP5 respectively, termed iFABP4 and iFABP5). We assessed their effects on MM cell apoptosis, cell cycle, cell number, gene expression and fatty acid metabolism. iFABP4 or iFABP5 demonstrated a dose-dependent decrease (using 0-150μM) in MM.1S, RPMI-8226 and OPM2 cell number over 72 hours of treatment via bioluminescence. Additionally, 50 μM iFABP4 or iFABP5 inhibit MM.1S cell growth in a time-dependent manner, and combination treatment of both inhibitors led to the greatest reduction in cell number. A flow-based analysis of MM.1S cell cycle revealed that co-treatment of iFABP4 and iFABP5 (iFABP4/5) led to a significant increase in G1 and a reduction in S phase, suggesting cell cycle arrest. Single treatment with either inhibitor led to a ~5% increase in apoptosis at 72 hours, and co-treatment resulted in ~10% increase via flow cytometry, suggesting that both increased apoptosis and cell cycle arrest contributed to decreased MM cell numbers. Results from RNAseq and Seahorse platform analysis of fatty acid oxidation changes are in progress and will be presented at the conference.
We next tested if iFABPs could enhance the efficacy of dexamethasone (dex), a common anti-myeloma treatment. Treatment of MM.1S cells with 80 μM dex led to a 3-fold increase in apoptosis, and combination with iFABP4 or iFABP5 led to significantly more apoptosis. The greatest increase in apoptosis occurred with the combination of iFABP4, iFABP5 and dex, which resulted in a 9-fold increase in apoptosis versus the vehicle. Similar trends were observed combining dex with iFABP4/5 on MM cell number, suggesting that combination treatments hold promise for MM patients.
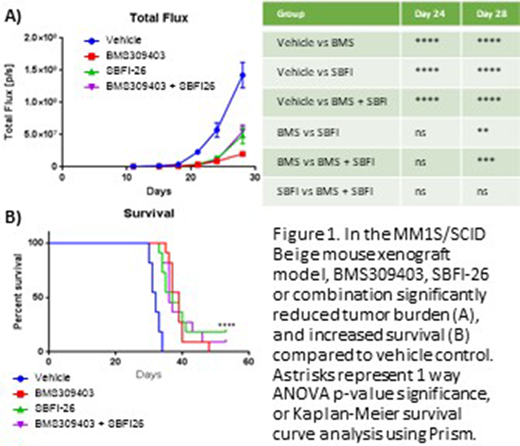
Finally, in vivo we tested the potential of targeting FABPs in a MM xenograft mouse model. Eight week old SCID-beige female mice (n=12) were inoculated with 5x10^6 human GFP+luc+MM.1S cells i.v, followed by iFABP treatments, initiated the next day. Treatments continued three times/week at 5mg/kg BMS309403, 1 mg/kg SBFI-26, or both, and mice were analyzed biweekly with live bioluminescent imaging of whole mice starting ten days post inoculation. As early as 21 days after MM cell injection, there was significantly lower tumor burden in all treatment groups compared to the vehicle, and this trend continued for the duration of the study (Fig 1A). The BMS309403 (iFABP4) treatment group had the least amount of tumor burden, and all 3 treatment regimens caused the mice to live significantly longer than the vehicle mice (Fig 1B). Our future studies will interrogate if effects on the tumor cells directly, and/or effects on the tumor microenvironment (eg. bone marrow adipocytes), caused these observed outcomes using FABP4/5-knockout or knockdown MM.1S cells and FABP4/5-/- genetic mouse models. We will also interrogate addition of dex and other MM drugs to the FABPi's. Collectively, this work suggests that FABPs are newly-identified targets pivotal for MM cell growth in vitro and in vivo and that inhibition of FABPs in vivo significantly improves mouse survival and decreases tumor burden. Thus, our research demonstrates a new, untapped therapeutic avenue for the treatment of MM patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.